
Did you know that over 21 million adults in the U.S. experience depression? This mental health condition is becoming increasingly common, even among children and teenagers.
Depression is characterized by persistent feelings of hopelessness, sadness, and a significant loss of interest in activities once enjoyed. These challenging emotions can profoundly impact a person’s quality of life.
It’s also observed that many individuals living with depression also experience Obsessive-Compulsive Disorder (OCD). This brings up an important question: can OCD actually cause depression?
There’s indeed a strong link between OCD and depression, with depression often arising as a consequence of living with OCD. The interplay between these two conditions can create significant difficulties for individuals.
Like depression, OCD can negatively affect daily life. The constant presence of OCD symptoms, such as intrusive thoughts and compulsive behaviors, can be incredibly distressing and, over time, frequently contribute to the development of depressive symptoms.
If you or someone you care about is showing signs of depression or OCD (whether separately or together), it’s important to seek understanding. While it can be tough for someone without a clinical background to untangle the nuances between these conditions, seeking professional help is crucial.
A mental health professional, such as a therapist, can assess your situation by asking relevant questions and evaluating your symptoms.
This blog aims to shed light on how OCD can lead to depression. We’ll also explore the symptoms of both conditions to help you gain a better understanding.
What is OCD?
You might hear people say, “I’m so OCD about that!” But what exactly is Obsessive-Compulsive Disorder?
OCD is a chronic mental health condition characterized by a pattern of recurring, unwanted thoughts and fears, known as obsessions. These obsessions often lead individuals to perform repetitive behaviors or mental acts, called compulsions. For example, if you’re preoccupied with thoughts about germs, you might feel compelled to wash your hands repeatedly to alleviate the distress those thoughts cause.
Living with OCD means experiencing this continuous cycle of obsessions and compulsions. It’s not typically a case of having one without the other; these two aspects usually occur together. For those who live with OCD, this cycle significantly interferes with daily life, often leading to considerable anxiety and stress.
What is Depression?
Feeling persistently sad or hopeless might indicate depression. But what defines depression as a mental health condition?
Depression is a mood disorder that deeply affects an individual’s emotional state. Those experiencing depression often describe waves of overwhelming sadness and hopelessness, carrying a heavy feeling that impacts their daily activities.
While it’s normal to feel sad or unhappy occasionally as a natural response to life events, depression involves sadness that is persistent and lasts much longer than usual.
If you’ve been experiencing prolonged feelings of depression, it’s important to consider seeking professional help. Leaving symptoms unaddressed can worsen the situation and further disrupt your daily life.
Symptoms of OCD
Let’s break down the common symptoms of Obsessive-Compulsive Disorder:
1. Obsessive Symptoms:
- A persistent need for symmetry, order, or perfection.
- Intense fear of losing, forgetting, or misplacing important items.
- Preoccupation with contamination or germs.
- Disturbing or unwanted thoughts, often involving taboo subjects like religion, sex, or harm.
2. Compulsion Symptoms:
- Repetitive mental rituals, such as silently repeating words or prayers.
- Excessive hand washing or cleaning.
- Repeatedly checking things (e.g., whether the door is locked or the stove is off).
- Arranging or organizing objects in a very specific, distinct way.
Symptoms of Depression
Now, let’s look at the symptoms often associated with depression:
- Thoughts of death or suicide.
- Overwhelming feelings of pessimism or hopelessness.
- Significant lack of energy, feeling slowed down, or persistent fatigue.
- Increased feelings of frustration, irritability, or restlessness.
- Sleep disturbances, including sleeping too much, having trouble falling asleep, or waking up too early.
- A marked decrease in interest or pleasure in activities and hobbies.
- A consistently sad, anxious, or empty mood.
- Difficulties with memory, concentration, and making decisions.
- Feelings of helplessness, guilt, or worthlessness.
Common Co-Occurring Symptoms of Obsessive-Compulsive Disorder and Depression
When Obsessive-Compulsive Disorder (OCD) and depression occur together, you might notice some overlapping symptoms. These can include:
- A significant loss of interest or pleasure in activities you once enjoyed.
- Intense distress or anxiety connected to specific thoughts or behaviors.
- Noticeable changes in your sleep and appetite patterns.
- Difficulty completing daily tasks, even those unrelated to compulsive behaviors.
- Persistent feelings of hopelessness and sadness.
Experiencing these symptoms can be incredibly draining and make everyday life challenging. When these signs become severe, they can significantly disrupt your routines, affect your relationships, and take a heavy toll on your overall mental well-being.
If you recognize these symptoms in yourself, it’s really important to seek help from a mental health professional. A psychologist can thoroughly assess your situation and work with you to develop effective strategies to manage these symptoms and improve your quality of life.
Can OCD Lead to Depression?
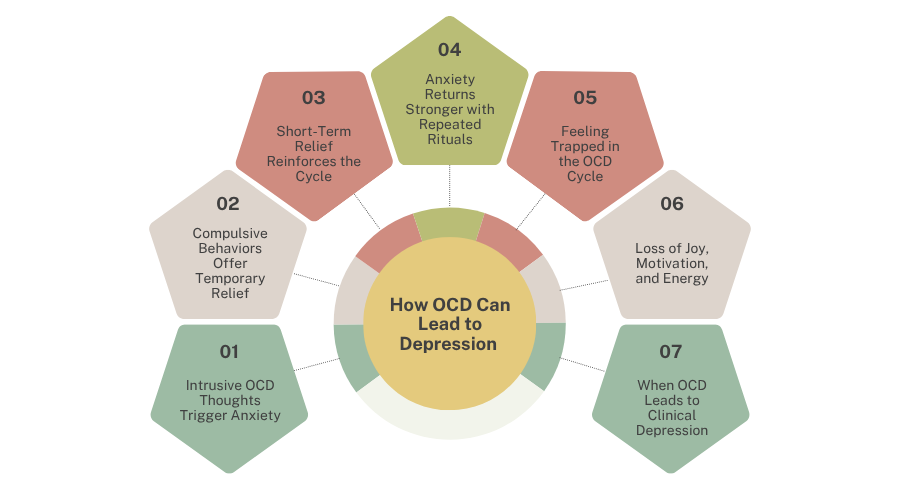
Many people wonder if there’s a link between Obsessive-Compulsive Disorder (OCD) and depression, specifically if one can cause the other. Let’s explore that connection.
It’s very common for individuals experiencing OCD symptoms to also develop symptoms of depression, and sometimes vice versa. However, when both conditions are present, it’s often observed that OCD symptoms appear before the onset of depressive episodes. This suggests that living with OCD can indeed contribute to the development of depression.
One common understanding is that depression can be a direct response to the immense challenges and distress caused by OCD symptoms. While the exact mechanisms are still being studied, mental health professionals often point to several ways OCD can lead to depressive states:
1. Strain on relationships and daily life
OCD can severely affect personal relationships and make everyday activities difficult, leading to social isolation and a diminished sense of purpose.
2. The burden of obsessions and compulsions
The relentless nature of intrusive thoughts and the need to perform repetitive compulsions create significant mental and emotional fatigue.
3. Extreme emotional distress
The sheer distress, anxiety, and shame associated with OCD can be overwhelming, eventually leading to a pervasive sense of sadness and hopelessness.
How Obsession and Depression Can Co-Occur
When you find yourself replaying the same negative thoughts repeatedly, this is known as rumination. Individuals with Obsessive-Compulsive Disorder (OCD) frequently experience persistent rumination, as their obsessions involve intrusive and repetitive thoughts.
This pattern of rumination is a key factor that can lead people with OCD to develop depression over time. Constantly having the same intrusive thoughts spiraling in one’s mind can inevitably lead to significant emotional distress, anxiety, and ultimately, a sense of hopelessness and sadness.
How Compulsions Can Contribute to Depression
The demanding nature of OCD compulsions can also contribute to the development of depression. People with OCD feel an overwhelming urge to perform specific behaviors or mental acts in response to their obsessive thoughts.
This need to perform rituals in a particular way is often tied to a quest for perfectionism, where individuals believe that if a task isn’t done “just right,” negative consequences will follow. This rigid adherence to rituals, such as repeatedly arranging items or performing actions in a specific sequence, is a core OCD symptom. However, the sheer time, effort, and frustration involved in maintaining these compulsions, coupled with the inability to achieve true “perfection” or lasting relief, can profoundly fuel feelings of despair and depression.
Can Depression Cause OCD?
Historically, researchers have noted the frequent co-occurrence of OCD and depression, often suggesting that the struggle to manage obsessive thoughts and compulsions could lead to depressive states. But this leads to another important question: can depression cause OCD?
Generally, clinical observations indicate that OCD symptoms tend to manifest before the onset of depressive symptoms. Individuals who struggle significantly with the intrusive nature of obsessions and the demands of compulsions often find themselves developing depression as a consequence of this burden.
While the precise causes of OCD are still being fully understood, several factors are recognized as potential contributors to its development. These may include:
- Certain infections, such as streptococcal infections (in some cases, like PANDAS).
- Genetic predispositions.
- Experiences of childhood trauma.
- Differences in brain structures, particularly within the frontal cortex and subcortical regions.
Currently, there is limited evidence to support the idea that depression directly causes OCD. However, the profound impact of untreated depression on mental well-being is undeniable.
Through a personalized therapy plan, mental health professionals can help identify the underlying causes of your depression. By using effective counseling techniques, they can support you in managing your symptoms and working towards a healthier, more fulfilling life.
How OCD and Depression Are Related?
The challenges of living with Obsessive-Compulsive Disorder (OCD) can unfortunately extend to affecting other aspects of mental health, often manifesting as depression. This is precisely why seeking professional help is so important if you’re experiencing OCD symptoms.
Individuals with OCD frequently grapple with persistent, intrusive thoughts that repeatedly spiral through their minds. This can lead to the development of rigid, often unchangeable behaviors or rituals (compulsions) that they feel compelled to perform. When these individuals are unable to act on their compulsions, or when their thoughts become overwhelming, it can cause a significant amount of distress.
This distress, stemming from the demanding nature of OCD, can manifest in various areas of a person’s life, significantly impacting their:
- Work performance
- Interpersonal relationships
- Overall life satisfaction
- Engagement in leisure activities
- Academic functioning
These widespread disruptions are a core reason why mental health professionals frequently observe a strong association between OCD and depression. In fact, many studies indicate that over 50% of individuals diagnosed with OCD also experience symptoms of depression.
The Interplay of Anxiety, Depression, and OCD
We’ve discussed how many individuals with Obsessive-Compulsive Disorder (OCD) also experience depression. But did you know there’s a significant connection between OCD, anxiety, and depression? Let’s explore how these conditions are linked.
When OCD goes untreated, the associated anxiety symptoms often intensify. This heightened anxiety, coupled with the ongoing struggle of managing obsessions and compulsions, can significantly contribute to the development of depression.
Leaving any of these conditions—OCD, anxiety, or depression—untreated can have long-term negative effects on the brain and overall well-being. Individuals who continue to manage their daily lives without addressing these symptoms may find themselves losing interest in activities they once enjoyed, struggling with executive functioning, and experiencing difficulties with attention and memory.
For instance, persistent anxiety can lead to feelings of guilt. If a person constantly feels guilty, this can become a deeply ingrained pattern, often leading to episodes of depression and a significant drop in self-esteem.
If anxiety symptoms are consistently affecting your daily life and well-being, it’s incredibly important to seek professional anxiety treatment. Addressing these concerns can prevent a cascade of further mental health challenges.
Similarities Between OCD and Depression
Individuals experiencing either Obsessive-Compulsive Disorder (OCD) or depression often share a tendency to fixate on negative thoughts, whether about the future or their perceived inability to control the present. From a biological perspective, the amygdala—a brain region crucial for emotional processing—may show heightened activity in response to significant distress, a state that can produce similar symptoms in both conditions.
Many symptoms of OCD and depression frequently overlap. These shared characteristics can include:
- Little to no satisfaction with life.
- Intense feelings or fear of failure.
- Frequent experiences of worry, hopelessness, or fear.
- Increased nervousness, agitation, or apprehension.
- Pervasive negative thoughts about oneself or engaging in negative self-talk.
- Persistent low mood and increased anger.
Differences Between OCD and Depression
While Obsessive-Compulsive Disorder (OCD) and depression can certainly be linked, they have fundamental differences that are important to understand.
Thought Patterns In depression, individuals are often preoccupied with pervasive negative thoughts and pessimistic beliefs, which usually stem from personal struggles or a general sense of hopelessness. These thoughts typically involve self-criticism or despair.
Conversely, with OCD, the core issue is obsessions—unwanted, intrusive thoughts that are often disturbing and feel alien to the person experiencing them. These thoughts vary greatly but are distinct from the general negativity seen in depression because they trigger intense anxiety and a need to perform a ritual.
Associated Disorders OCD belongs to a category of disorders that includes conditions like hoarding disorder, body dysmorphic disorder, skin-picking disorder (excoriation), and hair-pulling disorder (trichotillomania). While distinct diagnoses, they share common features related to repetitive behaviors or preoccupations that are different from typical depressive symptoms.
The Role of Compulsions A key differentiating factor is the presence of compulsions. People experiencing depression, even when battling negative thoughts, typically do not engage in repetitive physical or mental rituals to try and neutralize those thoughts. In OCD, however, compulsions are a defining characteristic: these are specific behaviors or mental acts performed repeatedly in response to an obsession, aimed at reducing distress or preventing a dreaded event.
Seeking Help and Treatment for OCD and Depression
Obsessive-Compulsive Disorder (OCD) and depression are prevalent mental health conditions that can leave individuals with persistent feelings of emptiness or hopelessness. To prevent these situations from worsening, seeking professional help is crucial.
After assessing your specific condition, therapists utilize various psychological approaches designed to reduce your symptoms and equip you with better coping strategies for triggers.
For depression, Cognitive Behavioral Therapy (CBT) is a widely applied and effective treatment. While some elements of CBT can be beneficial for individuals with OCD, a direct, unfiltered confrontation of OCD symptoms might not always be the most successful approach.
Instead, for OCD, more specialized forms of treatment are typically used. This often includes Exposure and Response Prevention (ERP), which is considered a gold standard therapy.
In cases where therapy alone may not be sufficient, healthcare professionals might also prescribe medications as part of a comprehensive treatment plan.
Now that we’ve explored the connection between OCD and depression, let’s understand how therapy uniquely addresses each condition.
Therapy for OCD
Individuals living with Obsessive-Compulsive Disorder (OCD) generally require a specialized treatment approach. Therapists primarily use Exposure and Response Prevention (ERP), which is considered the gold standard for OCD treatment.
While ERP is central, some elements of Cognitive Behavioral Therapy (CBT) can also be beneficial in managing OCD, particularly in milder cases or for those just beginning to show symptoms.
In ERP therapy, a mental health professional gradually guides individuals through a process of confronting their intrusive thoughts and fears. This involves carefully controlled exposure to situations or thoughts that trigger their obsessions, while simultaneously preventing them from performing their usual compulsive rituals. For example, therapists might guide clients through real-life scenarios, or if fears are more complex, they may ask them to vividly imagine the triggering situations. The goal is to help individuals learn that their feared outcomes don’t occur, even without performing compulsions, thereby breaking the cycle of anxiety and ritual.
If you suspect you have OCD, the crucial first step toward healing is finding a qualified therapist. Take time to research your symptoms and look for professionals who specialize in OCD and possess the necessary knowledge and skills to accurately assess your condition. It’s also important to find a therapist whose approach resonates with you.
You can seek a referral from your doctor, or you can independently research and find a therapist who fits your needs.
Therapy for Depression
For the treatment of depression, Cognitive Behavioral Therapy (CBT) is widely considered a primary and highly effective approach. During your sessions, a therapist will guide the conversation with thoughtful questions, but you’ll always have the space to initiate discussions about your feelings, behaviors, and thoughts when you feel ready.
This treatment plan is designed to help you understand the connections between your thoughts, emotions, and actions. If you’ve experienced a traumatic event in your past, your therapist will approach this topic with sensitivity and only explore it when you feel prepared to confront those memories.
Is it Possible to Have Both OCD and Depression?
Yes, it is entirely possible, and quite common, for individuals to experience both Obsessive-Compulsive Disorder (OCD) and depression. Research indicates that a significant number of people—estimates range from 25% to over 50%—who have OCD will experience depressive symptoms at some point in their lives.
Typically, individuals first develop OCD symptoms, with depression emerging later as a consequence of living with the distress and impairment caused by OCD. However, it’s also possible for symptoms of both conditions to appear simultaneously. While less common, there are rare instances where depressive symptoms might precede the onset of OCD.
Because of this common co-occurrence, it’s easy to mistakenly believe that depression is simply a component of OCD. It’s crucial to understand, however, that while they are frequently linked, OCD is a distinct disorder and not merely a symptom or subset of depression.
Dealing with OCD and Depression: A Holistic Approach
Both Obsessive-Compulsive Disorder (OCD) and depression are significant mental health conditions. While OCD often involves intrusive thoughts and compulsive behaviors, the distress these patterns cause can frequently lead to feelings of hopelessness and emptiness, mirroring symptoms of depression.
As we’ve explored, more than half of individuals with OCD will experience depression at some point, often with OCD symptoms appearing first. However, regardless of the order of onset, if you’re grappling with recurring negative thoughts, compulsive behaviors, or persistent anxiety and sadness, seeking professional help is a crucial step.
The journey towards a healthier mind and overall well-being can be challenging, but with proactive measures and the right support, positive change is absolutely achievable.
Our team, including mental health professional Dr. Alexandra Snead, is dedicated to supporting individuals through these complexities. Recognizing that the causes and manifestations of OCD and depression vary from person to person, we develop highly personalized therapy plans.
A fundamental part of our counseling process is ensuring you feel safe, heard, and understood. We are committed to providing a supportive and confidential environment where you can openly discuss your experiences. The more comfortable you feel sharing, the more effectively we can work together.
We utilize evidence-based therapy methods like Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP), tailored for children, teenagers, and adults. These approaches help individuals identify their triggers, understand their thought patterns, and develop more effective ways to manage their conditions.
Take the step towards positive change in your life—explore our mental health services today.

