
What Causes OCD to Get Worse and How to Regain Control? Do you ever find yourself checking the front door multiple times before leaving the house? Or feeling as though the same thoughts are looping endlessly in your mind? For many people, these experiences are more than habits. They may be signs of obsessive-compulsive disorder, commonly known as OCD.
Each day, millions of adults wake up to thoughts they cannot easily dismiss. OCD is a mental health condition characterized by persistent, intrusive thoughts that often do not reflect reality. These thoughts can feel overwhelming and disruptive, making it difficult to focus on everyday tasks.
As the mind fixates on distressing thoughts, people with OCD often turn to repetitive behaviors or mental rituals in an attempt to find relief. Over time, these actions can become ingrained patterns, commonly referred to as compulsions. While they may provide temporary reassurance, they often interfere with daily life.
What may begin as a small inconvenience can gradually become more disruptive. For example, repeatedly checking locks may cause delays at work or prevent someone from leaving the house comfortably. As intrusive thoughts increase, so do the challenges they create in real-world settings.
In many cases, OCD worsens without individuals fully understanding why. Learning how to recognize triggers and patterns is an important step toward regaining a sense of control. Working with a therapist can be especially helpful. In a supportive and confidential space, you can openly discuss your experiences and identify what contributes to symptom flare-ups. This understanding allows for the development of effective strategies to manage OCD more successfully.
In this blog, we’ll explore what causes OCD to intensify and share practical ways to manage these challenges.
What is OCD?
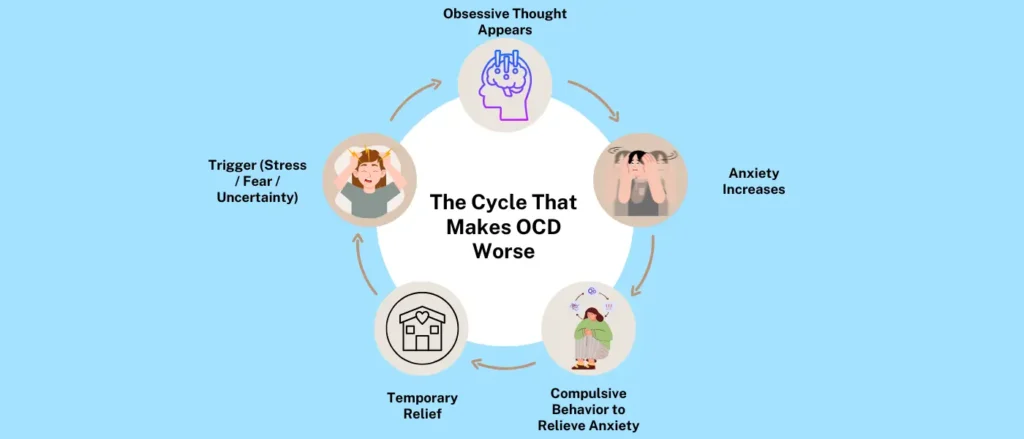
Obsessive-compulsive disorder is a condition in which unwanted, recurring thoughts lead to repetitive behaviors or mental acts. It often begins with a thought that feels intrusive or distressing. As attention becomes increasingly focused on that thought, it can turn into an obsession.
To relieve the anxiety created by these obsessions, a person may feel compelled to perform certain actions. These actions are known as compulsions. Many people experience a strong urge to complete these behaviors in a specific way or order, and not doing so can lead to significant anxiety or distress.
For example, someone with a fear of burglary may repeatedly check door locks to reassure themselves that their home is safe. Others may experience compulsions that are less visible. A person struggling with intrusive thoughts about harm may mentally count numbers or repeat phrases to neutralize the distress.
Even though these mental rituals are not outwardly noticeable, they can be just as exhausting and debilitating as physical compulsions. Most people with OCD are aware that their thoughts and behaviors are excessive, yet they often feel trapped in the cycle. Compulsions may bring brief relief, but they reinforce the obsession and keep the pattern going.
Without treatment, this cycle can intensify over time. With the right support, however, individuals can learn what causes their OCD symptoms to worsen and develop healthier coping strategies. A therapist can help identify triggers and guide treatment that reduces the impact of obsessions and compulsions, making long-term relief possible.
Signs of OCD
People living with obsessive-compulsive disorder often experience a combination of obsessions and compulsions. Obsessions are unwanted, intrusive thoughts, while compulsions are repetitive behaviors or mental acts performed to reduce anxiety. When someone feels unable to carry out these compulsions, distress and anxiety often increase.
While many people recognize their repetitive behaviors or persistent thoughts, they may not fully understand why they feel compelled to act this way. OCD can be confusing and frustrating, especially when the thoughts feel out of sync with a person’s values or intentions.
One of the earliest signs of OCD is excessive worry. These worries can become so intense and persistent that they turn into obsessions, dominating a person’s attention and daily life.
Common signs and symptoms of OCD may include:
- Fear of contamination from germs, bodily fluids, or dirt
- Feeling overly responsible for preventing harm or catastrophic events
- Intrusive thoughts about inappropriate or taboo behaviors
- Distressing thoughts about self-harm or fear of acting on unwanted thoughts
- Recurrent thoughts related to sexual orientation or gender identity
- Repeating everyday actions, such as standing up from a chair or walking through a doorway
- Excessive cleaning, such as frequent dishwashing or repeated handwashing
- Constantly checking the body for signs of illness despite reassurance
- Replaying or mentally reviewing events over and over
If these signs persist or interfere with daily functioning, it may be helpful to seek professional
support. Obsessive-compulsive disorder treatment takes place in a safe, structured setting where
you can explore thought patterns and behaviors with a therapist. With the right guidance, it is
possible to reduce symptoms and regain a greater sense of control over daily life.
What Makes OCD Worse?
When OCD symptoms are mild or moderate, many people begin to incorporate obsessions and compulsions into their daily routines. Over time, these behaviors can feel familiar or even manageable. Some people start to rationalize their compulsions, telling themselves that the behaviors are not harmful or that they serve a useful purpose.
As a result, individuals may become defensive about their actions and justify them as coping tools. When symptoms do not yet interfere significantly with work, relationships, or daily responsibilities, OCD may not feel like a serious concern.
However, as obsessive thoughts become more intense, compulsions often increase in frequency and visibility. These changes may be subtle at first and often become more noticeable during periods of stress. Even if others do not fully recognize what is happening, the internal distress continues to grow.
Several factors can contribute to OCD symptoms worsening over time.
1. Stressful Life Events or Circumstances
Stress is one of the most common triggers for OCD flare-ups. While stress affects everyone, people with OCD may experience a sharper increase in symptoms during major life changes, such as:
- Interpersonal conflict
- Moving to a new city
- Starting a new job or losing a job
- The death of a loved one
These events can disrupt routines, stability, and predictability, which are especially important for managing OCD. When that sense of structure is shaken, obsessive thoughts and compulsive behaviors may intensify.
2. Avoidance
OCD often creates a feeling of losing control, which can be deeply unsettling. To reduce anxiety, many people turn to avoidance as a short-term solution. For example, someone might think, “If I don’t leave the house, I won’t be exposed to germs.”
While avoidance may offer temporary relief, it tends to strengthen OCD over time. Avoiding feared situations prevents the brain from learning that discomfort can be tolerated. As a result, fears grow stronger and daily life becomes increasingly restricted.
Avoidance does not resolve obsessions or compulsions. Instead, it reinforces them and gradually shrinks a person’s world.
3. Reassurance Seeking
Questions like “Did I lock the door?” “Are my hands clean?” or “Am I a bad person?” are common for people with OCD. Seeking reassurance from others is often an attempt to relieve anxiety caused by intrusive thoughts.
Reassurance is a normal part of human connection. However, in OCD, it can become excessive. When loved ones repeatedly offer reassurance, it may soothe anxiety briefly, but it also reinforces the cycle of doubt. Over time, the brain becomes less able to tolerate uncertainty or discomfort on its own.
Although reassurance can feel helpful in the moment, it can unintentionally worsen OCD symptoms.
4. Isolation
Social withdrawal is common in many mental health conditions, including OCD. Social interactions may feel exhausting or anxiety-provoking, especially if certain situations trigger obsessions or compulsions.
People may begin avoiding friends, family, or social gatherings, not because they want to be alone, but because participation feels overwhelming. Instead of sharing their struggles, they may keep them private, which can increase stress and self-blame.
Isolation often leads to more rumination and emotional distress. Facing OCD alone can make symptoms feel heavier and more difficult to manage.
How Long Do OCD Flare-ups Last?
Once you understand what can cause OCD symptoms to intensify, it’s natural to wonder how long these flare-ups typically last.
OCD flare-ups can vary widely. For some people, symptoms may worsen for a few days, while for others, flare-ups can last several weeks or longer. The duration and intensity often depend on individual factors, such as stress levels, triggers, coping skills, and whether the person is receiving treatment.
Each flare-up follows its own timeline. In some cases, symptoms gradually ease as stress decreases or routines stabilize. In others, intrusive thoughts and compulsions may feel overwhelming and difficult to manage without support.
When flare-ups become intense or begin to interfere significantly with daily functioning, reaching out to a therapist can be an important step. Professional support can help individuals better manage obsessive thoughts and compulsive behaviors, reduce distress, and shorten the length of future flare-ups.
Methods to Manage OCD Flare-Ups
During an OCD flare-up, you may feel a strong urge to repeat everyday tasks in response to intrusive thoughts. For example, you might wash your hands frequently due to fears of contamination. While these behaviors may seem unnecessary to others, they often feel essential in the moment and can be easy to justify.
When compulsions remain mild and do not significantly interfere with daily life, people may learn to live around them. However, when symptoms intensify and begin to disrupt routines, relationships, or emotional well-being, it becomes important to actively manage OCD flare-ups.
Because OCD affects each person differently, effective management strategies vary. That said, therapy remains one of the most effective ways to reduce symptoms and prevent flare-ups from escalating. A therapist typically begins by identifying triggers and patterns, then develops a treatment plan tailored to the individual.
Below are two widely used, evidence-based approaches for treating OCD.
1. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy is a well-established treatment for OCD. It provides a supportive, nonjudgmental space where individuals can talk openly about obsessive and intrusive thoughts. A therapist works with the client to identify triggers, unhelpful thought patterns, and behaviors that maintain anxiety.
Once triggers are identified, the therapist introduces coping strategies to help manage flare-ups. For example, if anxiety increases before an important presentation and leads to compulsive behaviors such as skin picking, the therapist may recommend techniques like mindfulness, grounding exercises, or controlled breathing.
Practicing these skills helps reduce distress and shifts attention away from compulsions, making symptoms easier to manage over time.
2. Exposure and Response Prevention (ERP)
Exposure and Response Prevention is a specialized form of therapy commonly used to treat OCD. Similar to CBT, it involves discussing fears, triggers, and distressing experiences with a therapist. However, ERP focuses specifically on breaking the cycle between obsessions and compulsions.
In ERP, individuals are gradually exposed to feared situations in a safe, controlled environment. At the same time, they are supported in resisting the urge to engage in compulsive behaviors. Over time, this process helps the brain learn that anxiety can decrease on its own without rituals.
For example, someone with contamination fears may be guided to touch a doorknob and delay or resist washing their hands. While this can feel extremely uncomfortable at first, repeated practice often leads to reduced anxiety and increased confidence in managing symptoms.
With consistent support and practice, ERP can significantly reduce the intensity and frequency of OCD flare-ups.
Regain Control Over OCD with Snead Psychological Services
If you’re still wondering what causes OCD to worsen, the answer often lies in life changes and environmental stressors. Major transitions, interpersonal conflicts, or unexpected challenges can feel overwhelming and destabilizing. When this happens, intrusive thoughts may intensify and become harder to dismiss.
In response to these thoughts, compulsions often increase as a way to regain a sense of control. When symptoms remain mild, they may feel manageable. But as OCD becomes more severe, it can begin to interfere with daily functioning and emotional well-being. In some cases, untreated OCD can contribute to depression, social withdrawal, and difficulty completing everyday tasks.
Seeking professional support can make a meaningful difference. Therapy offers a space to understand what is happening, identify triggers, and learn healthier ways to respond to obsessive thoughts and urges.
At Snead Psychological Services, treatment focuses on helping individuals better understand their OCD and how it shows up in their lives. Dr. Alex Snead works closely with clients to identify patterns, uncover underlying triggers, and develop practical coping strategies. Because OCD looks different for each person, care is tailored to individual needs through personalized counseling.
In addition to OCD, services also support individuals dealing with anxiety, depression, tics, and related concerns. The goal is to help people feel more grounded, capable, and supported as they work toward a more fulfilling life.
If OCD is getting in the way of your daily life, support is available. With the right guidance, it is possible to regain control and move forward with greater confidence and clarity.
Frequently Asked Questions
1. Does stress make OCD worse?
Yes, stress can significantly worsen OCD symptoms. During stressful periods, intrusive thoughts often become more intense and frequent. In response, compulsive behaviors may increase as a way to reduce anxiety. These behaviors can show up as repeated checking, cleaning, or mental rituals that may be noticeable to others.
2. How severe can OCD become?
OCD can range from mild to severe, and in some cases, it can be highly disabling. When symptoms intensify, obsessive thoughts can dominate daily life and interfere with work, relationships, and overall well-being. To manage the distress, individuals may engage in repetitive behaviors that others may not fully understand.
3. What can trigger OCD?
OCD symptoms are often triggered or worsened by major life changes or ongoing stress. Common triggers include moving to a new city, relationship conflict, starting or losing a job, sleep deprivation, and chronic stress. These situations can disrupt routines and increase vulnerability to intrusive thoughts.
4. What are the side effects of OCD?
Living with OCD can be emotionally and physically exhausting. Common side effects include fatigue, disrupted sleep, irritability, and difficulty concentrating. Time-consuming compulsions can also make it challenging to manage daily responsibilities and maintain a sense of balance.
5. How can obsessive-compulsive disorder be treated?
Mild OCD symptoms may feel manageable at times, but when the condition begins to interfere with daily life, professional treatment can be very helpful. Therapies such as Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP) are widely used to treat OCD. These approaches help identify triggers, reduce compulsive behaviors, and build healthier coping strategies, making long-term symptom management possible.

