
Do you ever find yourself replaying old memories or overthinking the day the moment you lie down? Sometimes these thoughts can take over your entire night, leaving you wide awake and overwhelmed. You might even feel a sudden rush of emotion or the urge to cry as everything around you gets quiet.
Now imagine living with that feeling every night. You turn off the lights, hoping for rest, but instead of calm, a heavy wave of sadness settles in. By morning, the lack of sleep makes even the simplest daily tasks feel impossible.
Many people brush these experiences off or turn to quick, over-the-counter fixes. But when these patterns continue or worsen over time, they can be signs of something deeper.
You may be experiencing nighttime depression.
Nighttime depression is more common than most people realize. As your body moves through its natural circadian rhythms and the world becomes quieter, feelings of loneliness or emotional strain can intensify. For some, symptoms include fatigue, guilt, loss of interest, and difficulty falling or staying asleep.
If you notice these patterns, it is important to seek professional help. You deserve support, and nighttime depression can improve with the right care.
In this blog, we will explore the question many people ask: Why do I get so depressed at night? Keep reading to learn more about the causes, signs, and treatment options that can help you find relief.
Why is Depression Worse at Night?
Nighttime depression is a mood concern that can disrupt both your mental health and your natural circadian rhythm. For many people, it shows up through changes in sleep patterns and an emotional heaviness that becomes more noticeable after sunset.
As the evening arrives, you may feel a wave of sadness, hopelessness, or anxiety washing over you. These emotions can interfere with your sense of calm and make it difficult to fall or stay asleep. When this cycle continues through the night, it can drain your energy and affect your mood the next day.
There are several reasons why depression can feel more intense at night:
- Feelings of loneliness often increase as the world becomes quieter.
- Changes or imbalances in cortisol and melatonin levels can influence mood after dark.
- The stillness that comes with nighttime can bring unprocessed worries to the surface.
- With fewer distractions, negative thoughts have more room to take over.
What may feel like a confusing, overwhelming sadness often has identifiable causes, and there are effective ways to manage it.
A helpful first step is understanding how depression and insomnia connect. Gaining clarity about both conditions can guide you in choosing the right therapeutic approaches and treatment options for your sleep and mental health.
Is There a Connection Between Depression and Insomnia?
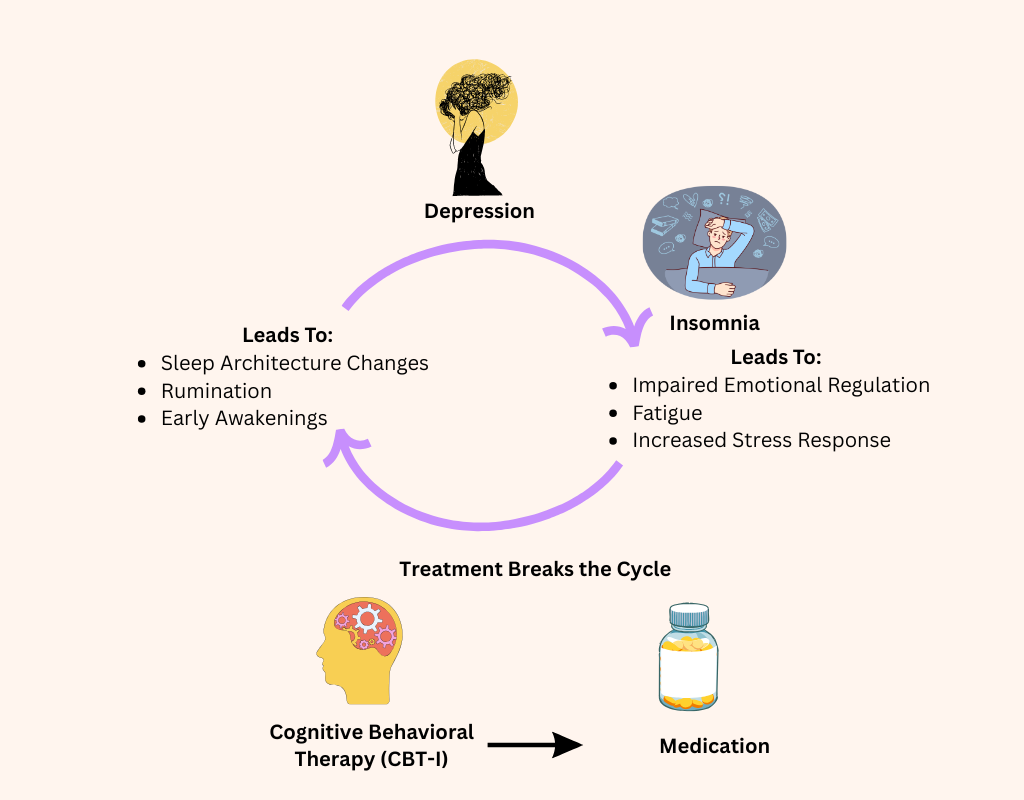
Yes. Depression and insomnia have a well-established, bidirectional relationship. Each condition can increase the likelihood of the other, and when they occur together, they can create a cycle that is difficult to break.
Research shows that about 40 percent of people with insomnia also experience depression, while nearly 80 percent of individuals with depression struggle with insomnia. Difficulty waking up in the morning is another sign that nighttime depression may be present. Many people with depression shift between insomnia and hypersomnia, moving from sleepless nights to periods of oversleeping.
Even everyday worries, such as concerns about finances, tension in relationships, or the stress of crowds and commuting, can cause nighttime wake-ups. Once awake, it can be hard to fall back asleep, which often adds irritation or emotional strain. It is also common to experience symptoms of both conditions at once, such as daytime fatigue, poor concentration, and low motivation.
Here are some important points about the depression–insomnia connection:
- Bidirectional relationship: These conditions influence each other. When one worsens, the other often follows, creating a continuous cycle.
- Insomnia increasing depression risk: Long-term sleep disruption affects emotional regulation and can heighten the risk of developing depression later in life.
- Depression causing insomnia: Depression often disrupts sleep quality and quantity. People with depression tend to have more difficulty falling asleep and staying asleep than those without mood symptoms.
- Shared vulnerabilities: Sensitivity to stress, emotional overload, and irregular sleep rhythms can contribute to both depression and insomnia.
Understanding how these conditions interact is an important step toward finding effective treatment and improving your overall well-being.
What are the Causes of Night Depression?
| Reason | Explanation | Effect at Night |
| Less Distraction | Daytime activities keep the mind busy; evenings are quieter. | More space for intrusive or negative thoughts. |
| Rumination | With fewer tasks, the mind replays stressful events or worries. | Increased sadness, anxiety, or emotional overwhelm. |
| Hormonal & Biological Factors | Melatonin increases and serotonin decreases at night. | Mood drops, vulnerability rises. |
| Unstructured Evening Time | Lack of routine leads to idle time. | More overthinking and emotional discomfort. |
| Loneliness & Isolation | Nights feel quiet; less social interaction. | Intensifies feelings of emptiness or sadness. |
| Fatigue | Tiredness reduces emotional resilience. | Problems feel heavier or harder to manage. |
| Poor Sleep Quality | Depression interferes with sleep, and lack of sleep worsens depression. | Creates a cycle of low mood and exhaustion. |
Have you ever asked yourself, Why do I get so depressed at night? You may already have a sense of what triggers it, or you might just feel that something is “off” as soon as the evening arrives. Nighttime depression can stem from several different sources. Some are easier to adjust or manage, while others may feel more difficult to control.
Often, nighttime depression is connected to what happens during the day. It can also be linked to disruptions in your body’s internal clock. Below are some of the most common reasons behind feeling low at night or experiencing insomnia followed by daytime fatigue.
1. High Stress
When you are overwhelmed by chronic stress or burnout, your evenings may feel anything but peaceful. You might notice a growing sense of hopelessness when stressful situations continue for long periods. By nightfall, the idea of waking up the next morning with a calm mindset can feel unrealistic. Over time, this pattern becomes familiar, and staying awake late into the night becomes a habit. Prolonged stress can significantly contribute to nighttime depression.
2. Rumination
Do you find yourself replaying events or worrying about responsibilities after the sun goes down? Depression often fuels negative thinking, making it easy to dwell on past mistakes or imagine worst-case scenarios. Rumination can spiral into anxiety, restlessness, and insomnia. While some reflection is normal, it becomes harmful when it begins to interfere with your daily functioning. Even the thought of waking up and facing an uncomfortable situation can intensify emotional strain.
3. Light Exposure at Night
Late-night screen time is one of the leading causes of disrupted sleep. Exposure to artificial light from phones, tablets, or TVs interferes with melatonin production, the hormone that signals your body to wind down. When your brain perceives this light as daytime, it delays sleep and increases mental strain. Over time, this disruption can affect mood regulation and contribute to nighttime depression.
4. Circadian Rhythm Disruption
Your circadian rhythm manages physical, mental, and behavioral cycles in a 24-hour period. This internal clock, controlled by the suprachiasmatic nucleus in the brain, responds to light and darkness. Any disturbance to this rhythm—such as jet lag, inconsistent sleep schedules, or working night shifts—can increase your risk of developing depression or struggling with nighttime wakefulness.
5. Chronotype
Your chronotype reflects your natural preference for feeling alert, productive, or tired at different times of the day. People generally fall into three categories: morning types, evening types, or somewhere in between. Morning types thrive early in the day, while evening types are more active later. Research suggests that evening types may have a higher likelihood of experiencing depression. Those in the “neither” category show moderate risk for sleep challenges.
6. Loneliness
Feelings of loneliness can intensify depression at night. This is especially common among middle-aged and older adults, but anyone can experience it. Even when surrounded by family or friends, emotional isolation can persist. When loneliness and stress combine, your body may stay in a heightened state of alertness, making restful sleep more difficult and increasing vulnerability to nighttime depression.
What are the Symptoms of Nighttime Depression?
High stress and anxiety can contribute to nighttime depression, and the symptoms often show up both emotionally and physically. While these signs are similar to those of general depression, many people notice that their symptoms become more intense in the evening.
Recognizing the signs early can help you seek support sooner and prevent the condition from interfering with your overall well-being.
Common symptoms of nighttime depression include:
- Changes in appetite, such as eating far more or far less than usual
- Sleeping excessively during the day or struggling to wake up
- Losing interest in activities you once enjoyed
- Feeling sad, restless, or anxious at night
- Frequent headaches, stomachaches, or other pain that does not improve with treatment
- Persistent feelings of guilt, loneliness, worthlessness, or helplessness
- Difficulty completing basic daily tasks like showering or brushing your teeth
- Crying easily or feeling the urge to cry without a clear reason
- Thoughts about death or suicidal ideation
How to Cope with Depression at Night?
By now, you know that insomnia can increase the risk of depression, and depression can make sleep even harder. When emotions feel overwhelming and difficult to regulate, nighttime can become a particularly vulnerable time. Lack of sleep alone can intensify sadness, irritability, and emotional exhaustion, even in people who are not clinically depressed. That is why finding coping strategies that work for you is essential.
Lifestyle changes can make a meaningful difference, especially when paired with patience and consistency. While there are many ways to manage nighttime depression, it is important to follow your doctor’s treatment plan as your primary guide.
1. Improve Your Sleep Routine
Feeling depressed at night often goes hand in hand with an inconsistent sleep schedule. Start by paying attention to what triggers your nighttime distress. Small habits, such as staying up until you feel exhausted, can make symptoms worse over time. Instead, try to create a calming bedtime routine.
If you are not sleepy, opt for a quiet activity like reading. Make your room as dark and quiet as possible to reduce distractions. Eating dinner at least an hour before bedtime may also help your body wind down more naturally.
2. Limit Blue Light Exposure
Blue light from phones, tablets, and laptops suppresses melatonin, the hormone that helps signal sleep. Too much screen time in the evening can make falling asleep much harder.
Turning off your devices at least two hours before bed can be especially helpful. Using blue-light filters or night mode settings can reduce exposure and make late-night scrolling less tempting.
3. Focus on Positive Thoughts
Shifting your mindset can help calm your brain before bed. Simple positive practices, such as repeating self-affirmations or reflecting on moments of gratitude, can ease negative thinking patterns.
Engaging in hobbies like painting, reading, journaling, or playing an instrument can also lift your mood and reduce evening loneliness. Reaching out to a friend or loved one for connection can make this time feel less isolating.
4. Reduce Caffeine and Alcohol
Caffeine blocks the chemicals that help your body relax into sleep, and alcohol may help you fall asleep at first but disrupts sleep as it metabolizes.
Limiting caffeine in the late afternoon and evening can improve your sleep quality. If you drink alcohol, try to keep it moderate and avoid using it as a sleep aid, since it can worsen nighttime depression and cause fragmented sleep.
5. Practice Mindfulness and Exercise
Mind-body activities such as yoga, meditation, tai chi, and qigong can help reduce stress and promote better sleep. Light exercise like walking can also improve your mood and support long-term emotional health.
Relaxation techniques—progressive muscle relaxation, deep breathing, visualization—help calm the nervous system and reduce rumination. Incorporating small moments of self-care can build resilience and significantly ease nighttime depression.
6. Seek Professional Help
Managing nighttime depression on your own can be difficult. When both insomnia and depression are present, symptoms often worsen without treatment. Talking with a mental health professional can help you understand the root causes of your symptoms and begin meaningful recovery.
Cognitive Behavioral Therapy (CBT) is one of the most effective treatments. It helps you identify unhelpful thought patterns, address rumination, and develop healthier coping strategies. You may also find it helpful to learn about different therapy approaches so you can communicate your concerns clearly to your clinician.
With the right support, you can begin to regain control over your thoughts, improve your sleep, and rebuild emotional stability. Nighttime depression is treatable, and you deserve care that helps you feel better.
When Should You Consult a Medical Practitioner for Night Depression?
If you find yourself feeling depressed at night or lying awake worrying about worst-case scenarios, it may be time to reach out to a healthcare professional. For a clinical diagnosis, symptoms typically need to be present for at least two weeks. A medical provider can help determine whether what you are experiencing is depression, another mental health condition, or a physical issue affecting your mood.
While depression can feel overwhelming, it is treatable, and early support can make a significant difference. You should seek help from a mental health professional if nighttime symptoms begin to interfere with your daily life.
Consider reaching out for support if you notice any of the following:
- You struggle to enjoy activities that once brought you pleasure
- You feel unusually hungry or lose your appetite without clear reason
- You have ongoing difficulty focusing or completing tasks
- You experience withdrawal symptoms or skip prescribed medications
- You feel fatigued or sleepy throughout the day despite spending time in bed
- You notice sudden mood swings or persistent feelings of hopelessness
- Your symptoms continue for more than two weeks and disrupt your routine
- You experience thoughts of self-harm or suicide
- Lifestyle changes and coping strategies are not helping to reduce your symptoms
Get a Peaceful Sleep with Proper Guidance from Snead Psychological Services
If you have ever wondered, Why do I get so depressed at night? you now understand some of the common causes and what you can do to regain control. Depression can be invisible to others while still deeply affecting your inner world, especially when symptoms interfere with sleep.
When nighttime depression begins to disrupt your rest, reaching out for professional support is an important step. Early treatment can lead to faster improvement in both sleep and overall mental health.
A skilled therapist can help you manage nighttime depression, reduce distressing symptoms, and strengthen your emotional resilience. At Snead Psychological Services, we offer both in-person and virtual sessions designed to support you through insomnia and mood-related challenges.
Our evidence-based treatments address the underlying causes of nighttime depression. One effective approach is Cognitive Behavioral Therapy for Insomnia (CBT-I), which helps replace unhelpful sleep-related thoughts with healthy, sleep-promoting habits.
With our guidance, you do not have to navigate nighttime depression alone. We work with you to build a personalized treatment plan that supports better sleep, improved mood, and long-term well-being.
If you are ready to experience calmer nights and more peaceful mornings, schedule an appointment with Dr. Alex Snead today. This is your first step toward restorative sleep and a more balanced, positive outlook.

